PCI Therapy for CHD
Things To Know About Choosing The Right Heart Stent
Foreword
Coronary atherosclerotic heart disease (CAHD) is triggered by myocardial ischemia, hypoxia or necrosis, which are caused by coronary atherosclerosis. CAHD is the most common type of organ lesion caused by atherosclerosis.
Coronary arteries, including the left and right branch, deliver blood to our heart. Coronary atherosclerosis may affect the coronary arteries separately or at the same time, the degree of lumen stenosis and locations of lesions determines the symptoms and prognosis of ischemia. Myocardial blood supply was not affected when the stenosis was less than 50%. When the lumen stenosis exceed 50%~70%, in the case of exercise, tachycardia or excitement, the oxygen consumption of the heart will increase, which may cause temporary myocardial blood supply shortage and chronic stable angina pectoris, the blood supply to the heart will not be affected only when resting. Acute myocardial infarction (AMI) may occur when atherosclerotic plaques rupture and bleed, forming thrombi that block blood vessels.
Therapies for CAHD
1.Drug Therapy:
1) Drugs that reduce symptoms and improve ischemia: Beta-blockers, nitrates, calcium channel blockers, and metabolic enhancer;
2) Drugs that prevent myocardial infarction and improve prognosis: anti-platelet drugs (aspirin, clopidogrel, ticagrelor), beta-blockers, statins, ACEI or ARB drugs.

2. Interventional Therapy (PCI)
PCI has the advantages of simple operation, less trauma and rapid postoperative rehabilitation, and can rapidly achieve vascular reconstruction in emergency. The main benefit of PCI in patients with stable angina pectoris (CHD) is to relieve symptoms, and improve quality of life, according to the existing research results, the first choice for most patients with stable angina (CHD) should be medication, and for those who wish to maintain good exercise tolerance, PCI should be considered. Patients with unstable angina could improve the long-term survival rate though PCI as well; patients with non-ST elevated acute myocardial infarction, based on risk stratification, should consider strategies of early conservative treatment or the early intervention. For patients with ST- elevated acute myocardial infarction, PCI could effectively reduce the overall mortality, but factors such as the onset time, location of infarction and cardiac function still need to be considered.

3. Surgical Therapy:
Coronary artery bypass grafting (CABG) may be more beneficial for patients with diabetes mellitus, multivessel lesions, left ventricular dysfunction, multivessel lesions at the distal end of left main and proximal end of left anterior descending, and those who could not gain complete vascular reconstruction though PCI.

Types and selection of heart stents for PCI
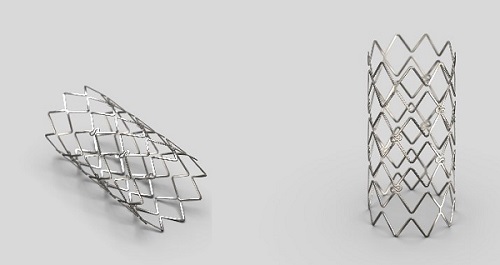
1. Bare Metal Stent (BMS) :
As a foreign matter planted in human body, bare metal stents will produce different stimulation effects after implantation. Due to the very nature of metal materials, problems such as metal corrosion, metal ion perpetuation in the body, activation of the blood coagulation system, regeneration of smooth muscle cells and deposition of cell substrate in the blood are inevitable. It may also trigger inflammatory responses in blood vessels, leading to blood vessel damage. According to statistics, the incidence of restenosis after BMS implantation is 20%~30%.
2. Drug Eluting Stent (DES)
On the basis of bare metal stents, drug coating and drugs (such as Sirolimus, Paclitaxel, and antithrombotic drugs such as heparin), antibodies or genes that inhibit intimal hyperplasia are added to the drug eluting stents. After stents implantation, drugs, along with the polymer coating, will be released in the target vessels to prevent the occurrence of restenosis.
(1) The first-generation DES—Durable Polymer Drug-Eluting Stent (DP-DES):
Reduced the rate of vascular restenosis (to 5%~10%). DP-DES realized controlled drug release, ensured the effectiveness of the stent, and also inhibit proliferation of vascular smooth muscle cells, improved resistance of stent thrombosis, increased the corrosion resistance of stents to prevent the dissolution of metal ions, and avoided complex blood, immune response and tissue reaction of patients with bare metal stents implanted. After implantation, the polymer coating may cause continuous inflammation of vascular wall and significant delay in endothelial healing, which may lead to increased risk of late and very late stent thrombosis. Long duration of DAPT therapy; and the high cost are the major shortcomings of DP-DES
(2) The second generation DES—Biodegradable Polymer Drug-Eluting Stent (BP-DES):
The new polymer coating could be completely degraded to CO2 and H2O in about 6 months after the PCI procedure, avoiding the inflammatory reaction caused by the polymer, thus reducing thrombosis and achieve early endothelialization. DP-DES could further reduce the incidence of stent restenosis; the period of taking DAPT drugs could be shortened to 6 months, reducing complications of bleeding and the costs.
The guidelines for percutaneous coronary intervention treatment in China (2016) recommended the use of new generation DES in direct PCI for patients with non-ST elevated acute coronary syndrome (I, A), ST elevated acute myocardial infarction (I, A), and CAHD complicated with diabetes (I, A) and chronic renal disease (I, B). The new generation of DES is also recommended for the following coronary artery lesions: ostial lesions (IIa, B), SVG lesions (I, A), and stent restenosis (I, A). For left main bifurcation lesions and CTO, priority should be given to the application of the new generation of DES to reduce the incidence of restenosis.
(3) Bioresorbable Vascular Scaffold (BVS) :
BVS includes scaffolds of natural biological material, synthetic polymer material and composite material. Prospect of BVS’ application is still lack of data support, and needs to be further studied.
LEADERS—A study on the two generations of DES
At the 2008 European ESC conference, the Late Breaking Trial session presented the results of LEADERS, a large sampled clinical trial comparing a new biodegradable polymer drug eluting stent (BP-DES) with the first generation durable polymer drug eluting stent (DP-DES).
The full study was published in the LANCET in 2011. This is the world's first large scale multi-center, head-to-head, randomized non-inferior clinical trial of the new and old generations of drug-eluting stents (DES), with sufficient sample size to ensure the effectiveness of the study. This trial randomly enrolled 1707 patients, whom are randomly and equally allocated to two groups. These patients have complex complications and lesions, including chronic stable coronary arteriosclerosis heart disease, acute coronary syndrome, diabetes mellitus, multivessel lesions and long lesions (> 20 mm), which made the sample resemble the real world clinical situation, and the results of the study in greater value to practical application.
The 9-month results showed that both the composite clinical endpoint (cardiac death, MI, TVR) and the angiographic endpoint (stent restenosis) reached the standard of non-inferiority and showed advantages in safety as well.
Summary
Although the first generation of DES has superior anti-restenosis advantages compared to BMS, the slight increase in the incidence of late and very late stent thrombosis has become another critical problem in clinical application, and may even become an important safety problem that hinders the development of DES. The technology of biodegradable polymer drug eluting stent (BP-DES),which was rapidly applied to new products from a concept, has gained more and more powerful evidence in a series of clinical trials, showing promising prospect.
Reference
1. Naruszewicz, M., [150 years of investigation of atherosclerosis--present status and perspectives]. Pol Arch Med Wewn, 1997. 97 Spec No: p. 37-45.
2. O'Gara, P.T., et al., 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv, 2013. 82(1): p. E1-27.
3. Martin, S.S., et al., 2013 ACC/AHA cholesterol treatment guideline: what was done well and what could be done better. J Am Coll Cardiol, 2014. 63(24): p. 2674-8.
4. Nishiyama, S., [Anti-anginal medication in management of acute coronary syndrome]. Nihon Rinsho, 2006. 64(4): p. 748-53.
5. Grobben, R.B., et al., Cardiac markers following cardiac surgery and percutaneous coronary intervention. Clin Lab Med, 2014. 34(1): p. 99-111, vii.
6. Bozikov, V., [Acute coronary syndrome in diabetes]. Acta Med Croatica, 2004. 58(2): p. 151-5.
7. Zain, M.A. and W.J. Siddiqui, Angioplasty, in StatPearls. 2018, StatPearls PublishingStatPearls Publishing LLC.: Treasure Island (FL).
8. Lee, J.Z., et al., Composite outcomes in 2.25-mm drug eluting stents: a systematic review. Cardiovasc Revasc Med, 2015. 16(4): p. 237-42.
9. Gundogan, B., et al., Bioabsorbable stent quo vadis: a case for nano-theranostics. Theranostics, 2014. 4(5): p. 514-33.
10. Stefanini, G.G., et al., Long-term clinical outcomes of biodegradable polymer biolimus-eluting stents versus durable polymer sirolimus-eluting stents in patients with coronary artery disease (LEADERS): 4 year follow-up of a randomised non-inferiority trial. The Lancet, 2011. 378(9807): p. 1940-1948.


